Is PEP right for me?
If you’re HIV-negative or don’t know your HIV status, and in the last 72 hours you
1. Think you may have been exposed to HIV during sex (for example, if the condom broke),
2. Shared needles and works to prepare drugs (for example, cotton, cookers, water), or
3. Were sexually assaulted, talk to your health care provider or an emergency room doctor about PEP right away.
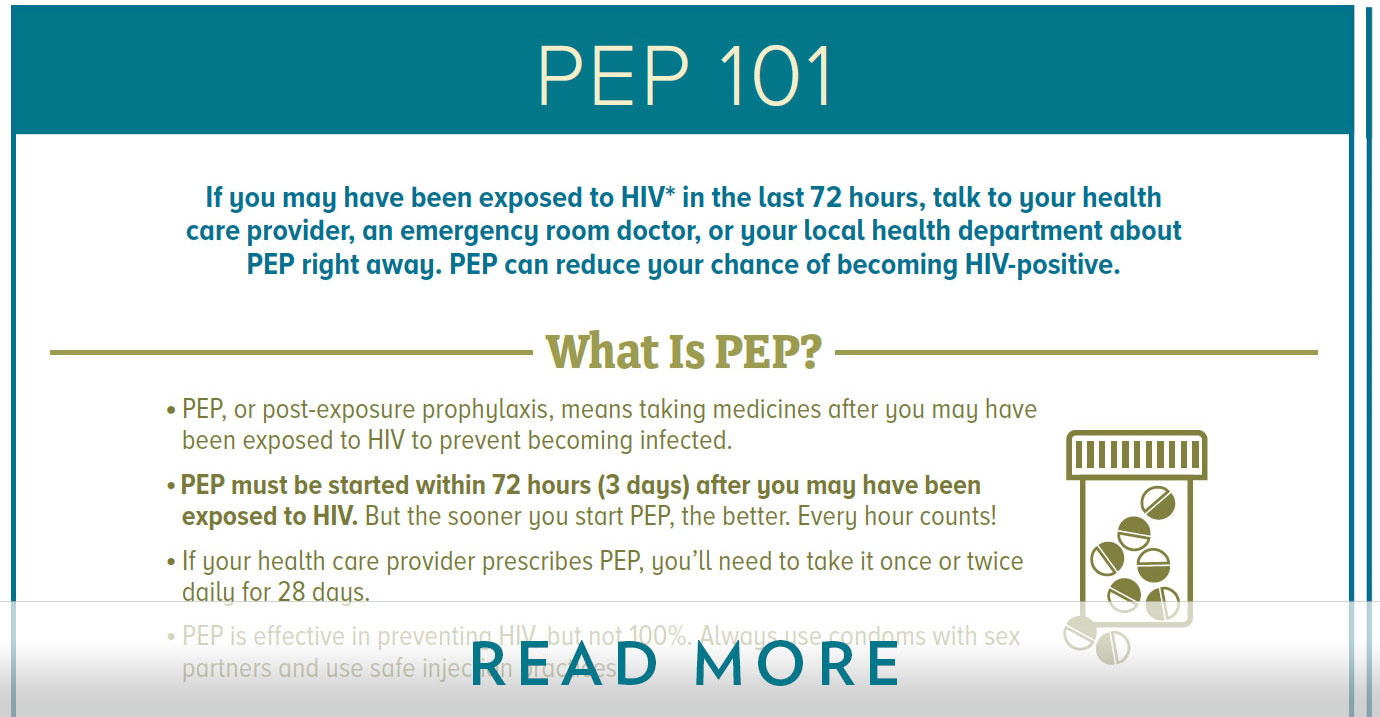
PEP should be used only in emergency situations and must be started within 72 hours after a recent possible exposure to HIV. It is not a substitute for regular use of other proven HIV prevention methods, such as pre-exposure prophylaxis (PrEP), which means taking HIV medicines daily to lower your chance of getting infected; using condoms the right way every time you have sex; and using only your own new, sterile needles and works every time you inject.
PEP is effective, but not 100%, so you should continue to use condoms with sex partners and safe injection practices while taking PEP. These strategies can protect you from being exposed to HIV again and reduce the chances of transmitting HIV to others if you do become infected while you’re on PEP.